Legal & Medical Brief: Why RI Courts Should Affirm that Natural Immunity in Youths Pre-empts Need for Vaccines
This brief was researched and developed to provide medical and legal analysis and recommendations with regard to the pending Nagle v. Nagle case in the Rhode Island Supreme Court.
Why RI’s Supreme Court Should Set National Precedent that Healthy Young Children with Naturally Acquired SARS-CoV-2 Immunity Don’t Need the Covid-19 Vaccine
by Andrew Bostom, MD, MS and Gregory Piccirilli, Esq.
On February 9, 2023, the Rhode Island Supreme Court (RISC) granted divorced father Joshua Nagle’s emergency motion for a stay on covid-19 vaccination of his young daughters, as petitioned via a lawsuit filed by his former wife. The RISC case was filed as an appeal to a previous ruling from Rhode Island’s Family Court, which sided with the mother.
When the RISC convenes to hear formal arguments in this case (Nagle v. Nagle), April 13, 2023, it will mark perhaps the first time in the nation that the matter of parental disagreement over childhood covid-19 vaccination is decided by a state’s highest court.
We believe the case of the father, Joshua Nagle, who seeks to avoid triple covid-19 vaccination of his healthy, previously SARS-CoV-2 infected five- and eight-year-old daughters, is firmly rooted in both evidence-based medicine and sound law.
The Evidence-Based Medicine Case Against Covid-19 Vaccination of These Previously SARS-CoV-2-Infected Healthy Five- and Nine-Year-Old Girls
Joshua Nagle’s daughters have been SARS-CoV-2 infected twice in the past ~year during January, and July, of 2022. Each time the girls were infected, they experienced either minimal symptoms, of brief duration, or were entirely asymptomatic. We now know those mild, self-limited SARS-CoV-2 infections confer a natural immunity to the virus that is more robust and enduring vis-à-vis any which might result from covid-19 mRNA vaccination. Key evidence in support of that contention, includes:
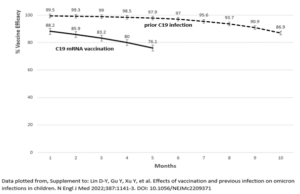
–North Carolina data from ~890K children aged 5 to 11 years-old during a period of SARS-CoV-2 omicron variant predominance (published in the New England Journal of Medicine) which revealed (see figure, below) the clear superiority of natural immunity in preventing covid-19 hospitalizations. Specifically, at 10-months, prior infection/naturally acquired SARS-CoV-2 immunity conferred 86.9% protection against hospitalization which exceeded the 5-month protection (76.1%) afforded by vaccination, with the gap widening each successive month (i.e., months 1-5) where direct comparisons were available.
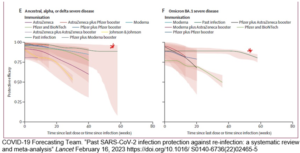
–A subsequent Lancet meta-analysis (figure follows) of adult populations confirmed and extended these findings demonstrating that prior infection afforded stronger, longer lasting immunity against “severe disease,” i.e., covid hospitalization and death.
–Subgroup data from Pfizer’s randomized, controlled trial (RCT) of covid-19 mRNA vaccination in 5 to 11 year-olds showed that among those children with prior SARS-CoV-2 infection, none even developed mild covid-19 infections in the either the active vaccine, or placebo vaccine groups.
Regardless of immune status, the SARS-CoV-2 infection fatality rate (covid-19 deaths/total infected) in children has been mercifully trifling, on the order of ~1/335,000 (0.0003%), globally, for those < 19 years-old.
More recent U.K. data evaluating the omicron variant period described a rate of 1/1,000,000 among 5 to 11 year-olds, while in children of all age groups, deaths were largely confined to those “with severe comorbidities, especially neurodisabilities.”
Rhode Island data provide local validation of these trends: there have been zero primary pediatric covid-19 deaths during 3 years of the pandemic
(here; here; The latter source also indicates there were 251 non-covid-19 pediatric deaths in Rhode Island from 1/1/2020-3/1/23). In contrast, three Rhode Island children died during a single pandemic H1N1 influenza season in 2009 to 2010.
Hospitalization rates, certainly for primary covid-19 hospitalizations (here; here), and in particular those with severe illness, have always been extremely low in children, since the advent of the pandemic. Moreover, concordant French and Canadian data reported pediatric influenza hospitalization rates for pandemic and/or select seasonal influenza years, were > 4-times those for covid-19. Again, data from Rhode Island are entirely consistent with these findings:
–During the 16-week period from February 13, 2022 through June 4, 2022 there were a total of only 15 primary covid-19 pediatric hospitalizations (for ages 0 to 17 years-old)—<1 per week—as determined by Rhode Island Department of Health (RIDOH) criteria;
–At the peak of this past “cold-flu season” in Rhode Island, i.e., October through December, 2022, there were 14 pediatric covid-19 hospitalizations, versus 67 pediatric influenza hospitalizations, and (at least) 304 hospitalizations for pediatric respiratory syncytial virus (RSV), per RIDOH (and Hasbro Children’s Hospital)
–For the past year (2/1/22 to 1/31/23), only six 5 to 9 year-old Rhode Island children have been hospitalized for primary Covid-19, irrespective of Covid-19 vaccination status (i.e., 2/ the 30-40% fully vaccinated; 4/ the 60-70% not fully vaccinated).
Rigorously and independently validating all these data, no child in either the placebo or actively vaccinated groups of Pfizer’s RCT of 5 to 11 year-olds was hospitalized.
These trial findings affirmed the very mild nature of covid-19 in children, and highlighted the complete absence of any RCT data—the highest standard of evidence (acknowledged in pediatric medicine as well)—demonstrating covid-19 vaccination of children “prevents” such rare covid-19 hospitalizations! Furthermore, there are literally no extant randomized, controlled trial data whatsoever evaluating “bivalent” covid-19 booster vaccination in children!!
Two peer reviewed assessments of covid-19 vaccination risk/benefit examining RCT data in low (i.e., confined to 18 to 29 year-olds) to moderate risk (i.e., all Pfizer and Moderna trial participants) have each demonstrated the risk of vaccine-associated serious adverse events (SAEs) outweighed any potential vaccine-associated reduction in covid-19 hospitalizations.
Given the extraordinarily low risk for covid-19 hospitalization in the pediatric population, relative to these adult populations, pediatric covid-19 vaccination risk/benefit stands, axiomatically, to be more adverse. Earlier we mentioned the paucity of covid-19 hospitalizations for Rhode Island children aged 5- to 9-years-old in the past year, only 6, divided in equal proportions, between those fully vaccinated and not fully vaccinated.
The Center For Disease Control and Prevention (CDC)’s passive vaccine injury surveillance mechanism, VAERS (Vaccine Adverse Event Reporting System), notoriously under-reports putative vaccine-associated adverse events (by ~30-fold in this peer reviewed study).
Two covid-19 vaccine-associated SAEs were recorded in VAERS among 5- to 9-year old Rhode Island girls during 2022, both requiring emergent care: a 5- year-old who presented with hives, and then a facial nerve palsy within 5-days of vaccination, and a 9-year-old who developed both chest pain/tightness, and hives, almost immediately after vaccination.
While the 9-year-old’s rapid-onset chest symptoms are clearly not consistent with covid-vaccine-associated myopericarditis (14 cases of which occurred during 2021 among healthy Rhode Island men under 35 years-old, and were published in a peer reviewed journal), we note the Taiwanese government just compensated the family of an unidentified 5- to 11-year-old girl who died from fulminant, autopsy-proven lymphocytic myocarditis 3-days after receiving the second dose of the Pfizer-BioNTech covid-19 mRNA vaccine.
Perhaps some of these unfavorable risk/benefit data have captured the attention of the vast preponderance of Rhode Island parents, only 36% of whom have chosen to vaccinate their 5-9-year-old children with the primary (2-shot) covid-19 vaccine series, while a mere 10% have “boosted” them with a third injection. Joshua Nagle shares the rational, evidence-based concerns of this super-majority 90% of Rhode Island parents who have decided they do not want their healthy 5- to 9-year-olds to receive three covid-19 vaccine injections.
Finally, the views of Mr. Nagle, and the lion’s share of Rhode Island parents, are externally validated by whole Western European nations, and America’s third largest state, Florida:
—France has just announced it is not recommending further covid vaccination for those under 65-years-old without comorbidity.
—Denmark does not recommend vaccination for any healthy persons under 50-years-old.
—Norway and Sweden do not recommend vaccinating healthy children under 18-years-old.
—The U.K. won’t even offer the vaccine to those < 12-years-old.
—Florida (already in March, 2022) recommended against vaccinating healthy children 5-to 17-years-old.
The Specific Legal Case Against Covid-19 Vaccination of These Previously SARS-CoV-2-Infected Healthy Five- and Nine-Year-Old Girls
We believe examination of the plaintiff’s pediatrician expert witness, Dr. Colleen Ann Powers, elucidated her non-evidence-based justification for vaccinating healthy, previously SARS-CoV-2 infected children, in our case, the Nagle children. We also maintain the Family Court trial judge’s decision in favor of the plaintiff was subject to contradictory legal reasoning.
Dr. Powers, the plaintiff’s pediatrician, recommended that the Nagle children, notwithstanding their naturally acquired immunity, receive the 2-shot original covid-19 vaccine series, and within 3-4-months afterward, also get a bivalent booster (third injection). She conceded that the sole purpose of the vaccine was to benefit the recipient by protecting against severe covid-19 illness, and death.
The only basis for her opinion that the Nagle children should receive the vaccine (X 3) was her incurious, uncritical acceptance of the generic recommendations of the CDC, and the American Academy of Pediatrics (AAP). She conducted no independent research; in fact, she was confused about when the Pfizer RCT in 5- to 11-year-old children was conducted, and what it had shown (i.e., no protection against covid-19 hospitalization could be demonstrated because there were no hospitalizations in the entire RCT, regardless of vaccination status, and not even the occurrence of mild infections amongst those children with prior natural immunity, also independent of vaccination status).
Dr. Powers was also unaware that the vaccine was only Emergency Use Authorized (EUA) but conceded that if POTUS Biden declared the emergency over, it might change her recommendation. (Note: On January 30, 2023, President Biden advised Congress that he will end the national emergency for COVID-19 on May 11, 2023. At present, it is unclear how that action will affect covid-19 vaccine availability, subsequently.)
Dr. Powers was further unaware that less than 40% of children in the US have had the vaccine (just 36% in Rhode Island have been vaccinated with 2-shots), even though those data are published in the AAP material she receives. She also did not know how many children in Rhode Island have died because of Covid, and was surprised to learn that number was zero.
As for whether the vaccine is required to attend school, Dr. Powers admitted it is not. She also agreed that in August, 2022, the Rhode Island Department of Education ended any distinction between covid-19 vaccinated or unvaccinated children in school.
Dr. Powers initially asserted that there was scientific consensus recommending the vaccine to children; but was unaware that at least one large state (Florida), and entire Western European countries (France, the U.K., Denmark, Sweden, Norway), did not.
She was unaware that the infection fatality rate for COVID in 0- to 19-year-olds is 0.0003%, or that of those 3 deaths per million, virtually all occurred in children with major, chronic co-morbidities. When confronted with such irrefragable information, Dr. Powers admitted she was “surprised.”
Similarly, Dr. Powers downplayed evidence of potential harm as reported in the Vaccine Adverse Event Reporting System (VAERS). In September of 2021, the RIDOH produced a report (published in The Rhode Island Medical Society Journal) which noted that within the first eight months of VAERS surveillance of Rhode Islanders after the covid-19 vaccine rollout, between January and September of 2021, there were nearly 1,500 reports of vaccine-associated adverse reactions, including 89 hospitalizations, and 16 deaths.
When presented with this information, Dr. Powers tried to minimize it, although she did concede that “they (presumably, RIDOH) should investigate that.” (Unfortunately, despite repeated inquiries, we have not been able to uncover any evidence that RIDOH has followed up on that 2021 report.)
We argue, moreover, the Family Court trial judge, Associate Justice Sandra Lanni erred in two fundamental ways. First, she made a best interests of the child determination after finding that the father acted reasonably in accordance with the final divorce decree.
Second, even if the Family Court were permitted to ignore the language of the final decree, the Court (i.e., via Judge Lanni) failed to articulate how the 8 factors in the best interest of the child standard warranted a change in custody for the mother to make the sole decision regarding COVID-19 vaccination.
In addressing the final divorce decree and the issue of reasonableness, the Family Court found that “there is not uniformity of agreement in the medical community regarding whether children, in general, should receive the COVID vaccine and whether the benefits of the vaccine to children, in general, outweigh the risks or vice versa.” Further, she found that the parents generally agreed to all medical recommendations of the pediatrician, including other vaccines; the sole issue of dispute involved COVID-19. This led inextricably to the Family Court determining that the father had acted reasonably in rejecting the vaccine:
“In light of the evidence before the Court, the Court cannot conclude that the Defendant’s refusal to follow the recommendations of Dr. Powers, in this one instance, is objectively unreasonable.”
But then the Family Court overruled the father’s objection to the vaccine:
“To the extent that the Defendant argues that the language in the marital settlement agreement and in the final judgment means that if one parent has a reasonable objection to a recommendation of the children’s pediatrician, then that parent will automatically prevail, the Court rejects that argument. That language is not stated. It could have been stated, but it was not. Furthermore, the Court always has the jurisdiction to resolve issues relating to the minor children in a divorce if those children — if those issues relate to the children’s healthcare.”
The parties (i.e., the Nagle parents) used the language “neither party shall unreasonably withhold consent” in other sections in the final divorce decree, including, notably,medical and dental treatment. The Court should have ended its consideration of the case once it found the father acted reasonably. To do otherwise in essence rewrites the final divorce decree and overrules what the parties had agreed to.
When a party seeks to modify a custody order, there must be a showing of changed circumstances. Only then does the Court invoke the best interests of the child standard. Olson v. Olson, 701 A.2d 1030, 1031 (R.I. 1997). Since the Court here made no such determination of changed circumstance, Judge Lanni’s decision must be reversed.
Prior to conducting hearings on the matter, the Family Court asked the parties for any case law in other jurisdictions in which the issue here was presented. The parties were only able to find few mostly unpublished trial court cases. One, J.F. v. D.F., 160 N.Y.S.3d 551 (N.Y. Sup. Ct. 2021), is particularly inapt, in that the child there was old enough to express her desire to be vaccinated.
Dismissing the father’s concern as “wait and see what further research demonstrates on both the efficacy of the vaccine and the impact of both short and long-term side effects;” the Court there used hyperbole that the father’s position was, “untenable, when the specter of a killing or incapacitating disease is swirling in the environment surrounding this young girl.” This statement ignores the fact that young people are at practically zero risk of serious illness or death from Covid. The covid-19 vaccines are also non-sterilizing, and do not prevent transmission.
Another case is unpublished: Richmond v. Natanson (No. FD-14-49-15, Superior Court of New Jersey, June 24, 2022). In that case, the Court heard from both parents, as well as expert witnesses for both. The trial judge made extensive findings of fact based upon the relevant 11 factors for the best interests of the child under New Jersey law. First, the Court found that many of the factors did not skew either way; both parents were fit and cooperative and in agreement with all medical decisions except the COVID-19 vaccine. In finding that the child should be vaccinated, the Court relied heavily on the following facts: that the “continuity and quality of the minor child’s education would be disrupted by virtual learning, which would be more likely to occur if the minor child is unvaccinated.” Also, the Court found the minor child’s daily life would be adversely affected if she remained unvaccinated. Most importantly, the Court found that the child had not been previously infected and had no natural immunity. In making that determination, the Court also relied on the testimony of the mother’s expert witness, a professor of pediatrics and infectious diseases, over that of the father’s expert who was in general pediatric practice.
At the close of this case, in Family Court, we noted to the Court that these factors, which led the New Jersey Judge to rule in favor of the vaccine, now skew heavily to the father’s position. First, the Family Court agreed that the father was a fit parent and cooperative and the COVID-19 vaccine issue is the only medical issue on which the parents disagreed. Second, the children here have both had covid and therefore have natural immunity. Moreover, there was no evidence that the children’s unvaccinated status had any effect on their daily living. And finally, the father’s expert demonstrated himself to be far more qualified to opine on the necessity of the vaccine than the children’s rather uninformed pediatrician.
Ultimately, Judge Lanni found none of the cases cited helpful, and ignored them. Yet, she then made no effort to even identify which of the best interests of the child factors favored overruling the father’s reasonable objection to the treatment. While the Rhode Island Supreme Court gives deference to best interests’ determinations made by a trial judge, a parent moving to change custody must, “show by a fair preponderance of the evidence that circumstances had changed such that the placement should be modified in the interest of the children’s welfare and that the change of placement was in the best interests of the children.” Souza v. Souza, 221 A. 3d 371, 377 (R.I. 2019). Where the Family Court fails to make a finding of substantial change in circumstances before considering the best interests of the children, the Supreme Court should reverse.
We maintain the automatic stay granted by the Rhode Island Supreme Court should remain in effect during the appeal where there is no finding that the children will suffer irreparable harm by remaining unvaccinated against COVID-19.
In March of 2022, a Court in Ontario, Canada ruled that a father who had final decision-making authority over medical decisions should not lose that right because he disagreed with the COVID vaccine for his daughter. The Judge noted:
“We are currently in a dynamic and rapidly changing situation in public health advisories concerning the COVID-19 situation, particularly concerning children.” A.M. v. C.D., 2022 ONSC 1516, p. 12 (March 9, 2022).
A year later this statement is truer. The covid-19 pandemic is over. The irrefragable evidence is that these children are at no risk of harm from severe covid-19 illness, that those with natural immunity are at least as protected as those who have had the vaccine, and that there are serious questions as to the harms that the covid-19 vaccine may cause. To the extent the Rhode Island Supreme Court wishes to continue this case to the full briefing calendar, the balancing of risks favors continuing the stay of any administration of the vaccine.
CONCLUSION:
Given the corpus of medico-legal evidence we have amassed, we recommend that the Rhode Island Supreme Court, to rule on behalf of the father, to reverse the decision of the Family Court and dismiss the mother’s motion, or at least place this matter down for full briefing, while maintaining the stay of the lower court decision.
About the authors:
Dr. Andrew Bostom is an academic internist, clinical trialist, & epidemiologist at Brown University Medical School for 24-years (now retired). As an adjunct scholar to the RI Center for Freedom & Prosperity Bostom has been at the forefront of the international effort to raise awareness about the truth of the medical data regarding Covid-19 mandates.
Gregory Piccirilli is a private practice attorney, affiliated with the Flanders Legal Center for Freedom, and has served as primary and local attorney for multiple Covid-19 related civil rights cases.



